Robotic Vasectomy Reversal
You’ve probably noticed many advertisements, even billboards, showing the ease with which vasectomies can be performed. This is true. A vasectomy is a relatively straightforward procedure requiring little downtime and minimal pain. If you would like to learn more about a vasectomy, we suggest you read our article.
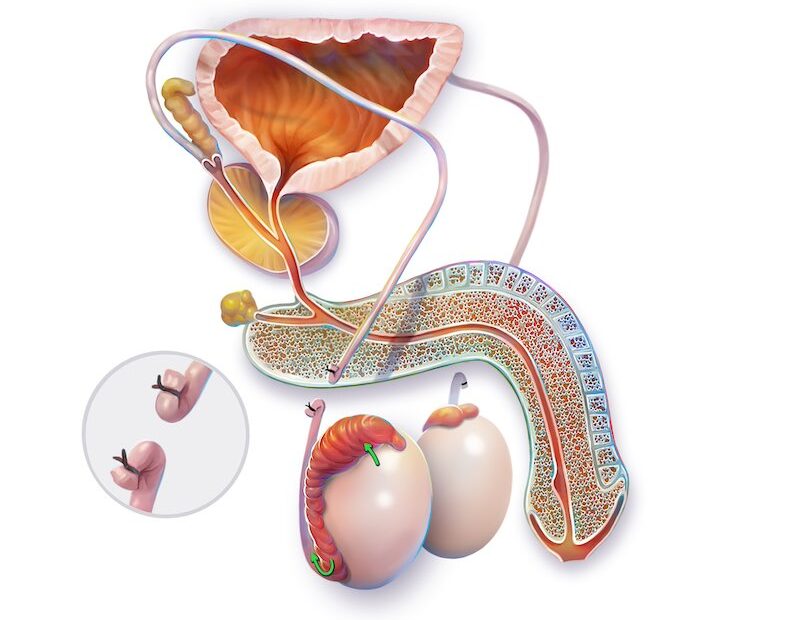
A vasectomy reversal, however, is more involved and requires additional considerations. However, it is certainly possible, and Dr. Engel is amongst a small number of surgeons performing this procedure regularly in the DC, Maryland, and Virginia areas. Although different techniques are used, ranging from open or no scalpel, cautery or no cautery, clips or stitches, a vasectomy is always the act of severing the tube (the vas deferens) that carries sperm from the testicle to the ejaculatory duct in the prostate. A vasectomy reversal likewise can be done via different techniques but always refers to the reconnection of the vas in a way that re-establishes patency of the sperm plumbing and the hopeful resolution of sperm flow. Literature has shown that a microsurgical connection done either by hand under a microscope or using robotic surgical instruments to perform microsurgery yields a higher patency rate, and these two options make up the vast majority of vasectomy reversals today.
Why Do Men Want a Vasectomy Reversal?
Vasectomy reversal candidates most often come to us with changes in their lives. By some estimates, these patients account for about 10% of all men who have undergone a prior vasectomy. Some, after thinking they were done having children, want more. Others may have remarried and are looking for a biological child with a new partner. The reasons are many and varied; however, patients who believe their ability to have children after a vasectomy is compromised or even ruined by having a vasectomy are usually happy to hear that, in most cases, that is not true.
What Are The Options?
There are always options, and all are reviewed during an initial consultation. The key point is that the testicle will continue to make sperm indefinitely even though the vas deferens has been blocked. Ultimately, the goal is to receive sperm that will allow for fertilization. Of course, we would consider achieving that via allowing that sperm to come from a penis during intercourse optimal, but other options do exist. With the standardization of in vitro fertilization, the other option is to retrieve sperm via extraction from the sperm plumbing (the epididymis) closer to the testicle via needle extraction or even using actual testis tissue to find an immature sperm that could be used to fertilize an egg. Considerations that might cause one to lean either towards or away from vasectomy reversal versus a fertility center using in vitro fertilization is, at times, cost (sometimes IVF is covered and vasectomy reversal is not), age of the wife/partner, time since the vasectomy which can adversely affect success rate of vasectomy reversal or just personal preference.
How Much Does Vasectomy Reversal Cost?
One thing that we know is always a consideration here is the expense a vasectomy reversal will bring. We are keenly aware that expense is often the sole determinant of whether someone would proceed or not with vasectomy reversal. We will first, of course, see if there is insurance coverage with your carrier for you, but if not, we have chosen Reston Hospital to be the most economical site that has given a special rate to use their operating room and robot. In doing this, and in Dr. Engel keeping his fee to a minimum, we seek to help as many patients as possible for a cost certainly well below the national average.
What Does a Vasectomy Reversal Entail?
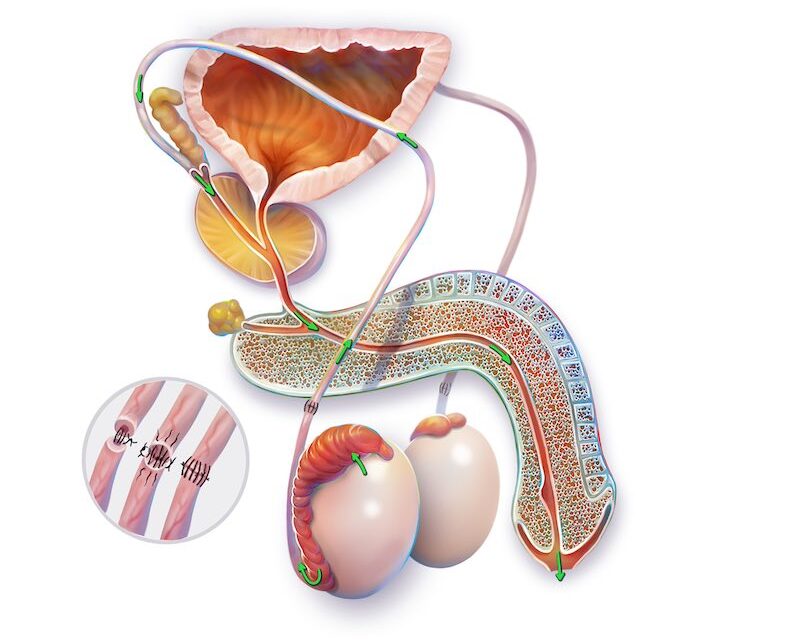
Vasectomies can be reversed using one of several techniques, but two approaches tend to yield the best results: the standard microsurgical technique and the robotic approach. Both procedures involve the same basic concept – taking the divided ends of the vas deferens and microscopically reattaching them with tiny sutures with three separate layers of sutures. At times, to find patency of sperm fluid flow, we must attach the vas directly to the epididymal tubules near the testicle. Connecting the two ends of the vas is called a vasovasostomy, and connecting the distal vas to the epididymis is called a vasoepididymostomy.
These procedures take two to four hours in both cases and offer excellent results. Vasectomy reversals are done via small incisions on both sides of the scrotum that are not much larger than the original vasectomy sites, with recovery and pain afterward also quite similar in scope and time course. Far more emphasis is made on refraining from extensive exercise or sexual activity until all pain has gone away in 2-3 weeks.
A Robotically Assisted Procedure
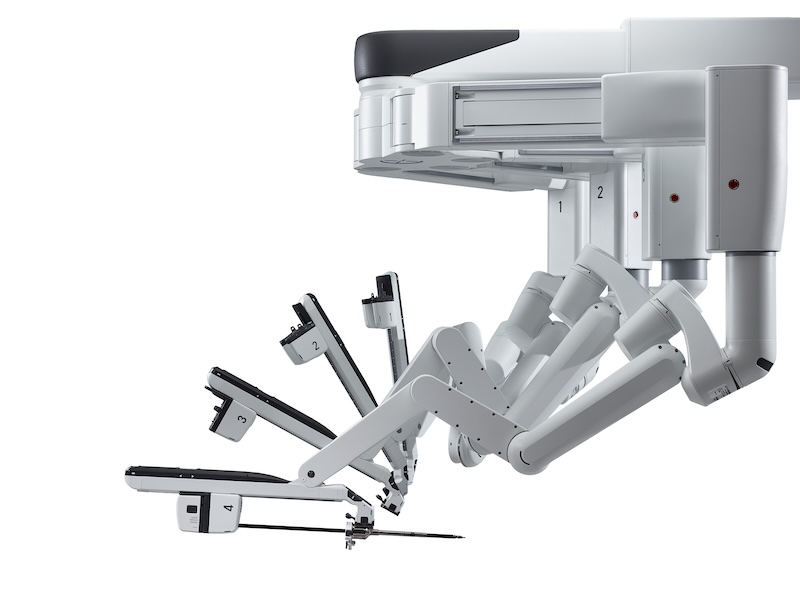
Dr. Engel has explored the use of robotic assistance in reducing operative time and even improving results. The traditional microsurgical vasectomy reversal is a demanding procedure that requires a great deal of effort and microsurgical expertise on the surgeon’s part. Fatigue in working with such small sutures is common under the microscope, and the unavoidable presence of hand-tremor can be very frustrating and limiting. However, robotic assistance allows for increased visualization, precision, and surgeon comfort for surgeons who have mastered these tools.
The robot is designed to work with such small sutures, removes any hand tremors, and allows for easy ergonomics when performing this suturing. These are important factors in the procedure’s success and operative time. Ultimately, whether a microsurgical or robotic approach is used, both are certainly excellent ways to do this, and the approach used is typically a function of a surgeon’s experience. Dr. Engel shifted from the microsurgical to the robotic technique exclusively over five years ago.
Below, please find actual videos of Dr. Engel performing both a robotic vasovasostomy and also a robotic epididymostomy:
Robotic Vasovasostomy
This is footage of robotic vasovasostomy, a specialized surgical procedure that utilizes robotic assistance to restore fertility in men who have previously undergone a vasectomy. The advanced robotic platform provides surgeons with enhanced dexterity, precision, and magnification, allowing for the meticulous handling of the delicate vas deferens. You can see Dr. Engel’s control of the robotic arms to perform microsurgical suturing, reconnecting the ends of the vas deferens. The footage highlights the intricate dissection, the use of ultra-fine sutures, and the attention to achieving a watertight closure to maximize the chances of sperm passage. This technique has become increasingly popular due to its ability to improve surgical outcomes, reduce operating times, and ensure quicker recovery for patients.
Robotic Vasoepididymostomy
Robotic vasoepididymostomy is a complex microsurgical procedure performed to bypass an obstruction in the epididymis and restore the flow of sperm into the vas deferens. This procedure is often utilized for patients with post-vasectomy obstructions or congenital blockages. This actual surgery footage showcases the exceptional precision required, as Dr. Engel uses robotic instrumentation to delicately incise the epididymal tubule, locate motile sperm, and create a direct connection to the vas deferens. The robotic platform offers unparalleled magnification and fine motor control, enabling the surgeon to place ultra-fine sutures through the microscopic lumen of the epididymis and vas deferens.
How Successful Is a Vasectomy Reversal?
The success of a vasectomy reversal has everything to do with the proximity to the actual vasectomy, and we see men with all timeframes. Generally speaking, we give patients approximate success rates in different ranges. Those who had their vasectomy less than three years earlier have success rates of over 90%. Five to ten years earlier, closer to 70-80%. Ten to fifteen years, we quote 50-60%, and beyond that, perhaps 50% or less. Some things might be more suggestive of success, such as the presence of what is called a sperm granuloma or if the sperm plumbing is dilated proximal to the vasectomy. Testis atrophy or problems that occurred with the original vasectomy can be a negative sign.
What is certain is that at this stage of Dr. Engel’s experience curve, the quality of the reconnection will be excellent, such that the success or failure of the procedure will solely have to do with what is found at the time of surgery. There is always a sense of high anticipation as to what will be seen when the vas is opened and prepared for reconnection. Patients will know that three things will be seen in the OR when opening the testis side of the vas: cloudy fluid with sperm, which almost always yields success; cloudy fluid without sperm, which is also excellent; clear fluid that will yield 50/50 success or a toothpaste-like substance. In the lattermost case, this suggests that the tubules are simply not patent, which can either be from upstream obstruction or the testis’ complete failure. This is where a vasoepididymostomy is considered if dilated tubules in the epididymis are seen. Otherwise, a testis biopsy and the use of testis tissue would be the next step.
We cordially invite you to visit Dr. Engel as an initial consultation to explore your options tailored to your specific situation and how we may best help you.